Table of Contents
Welcome to our comprehensive guide on tubal ligation. In this blog post, we explore the various aspects of this surgical procedure, including the risks and alternatives as well as answer the question, “How much does it cost to get your tubes tied?”
In order to help you make an informed decision, we will also discuss the factors that affect the cost and what to expect before, during, and after the procedure. So, let’s dive in and explore everything you need to know about tubal ligation.
Introduction to Tubal Ligation
Definition of Tubal Ligation
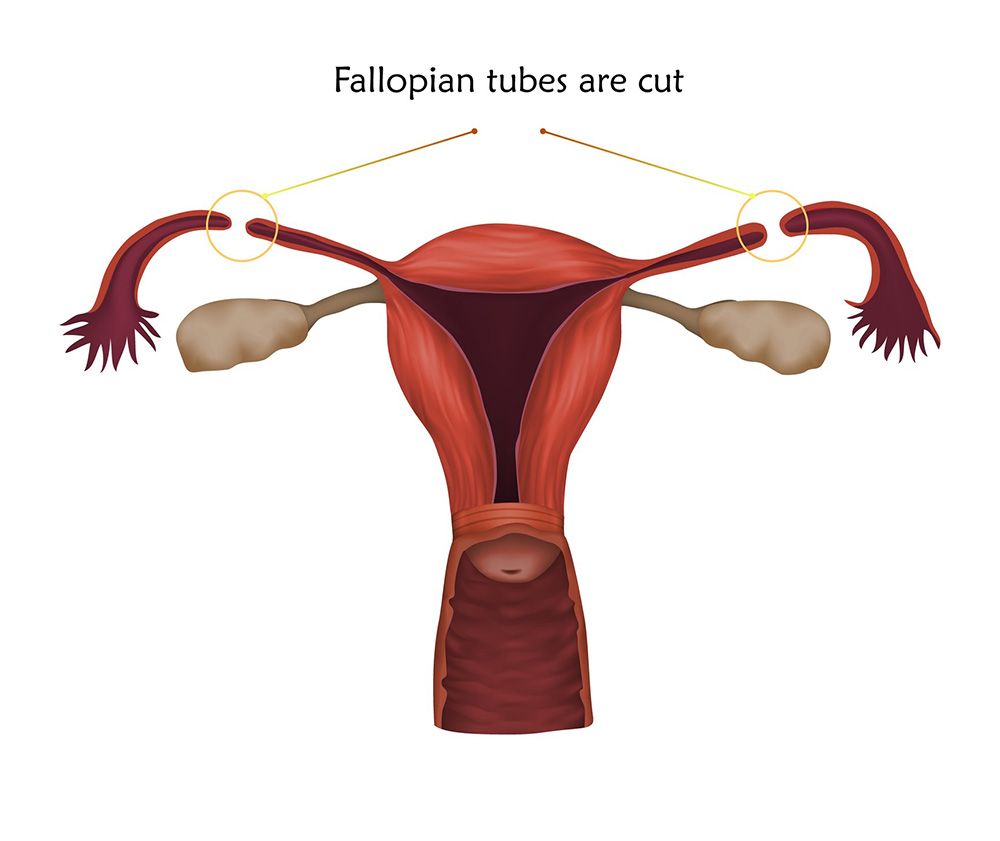
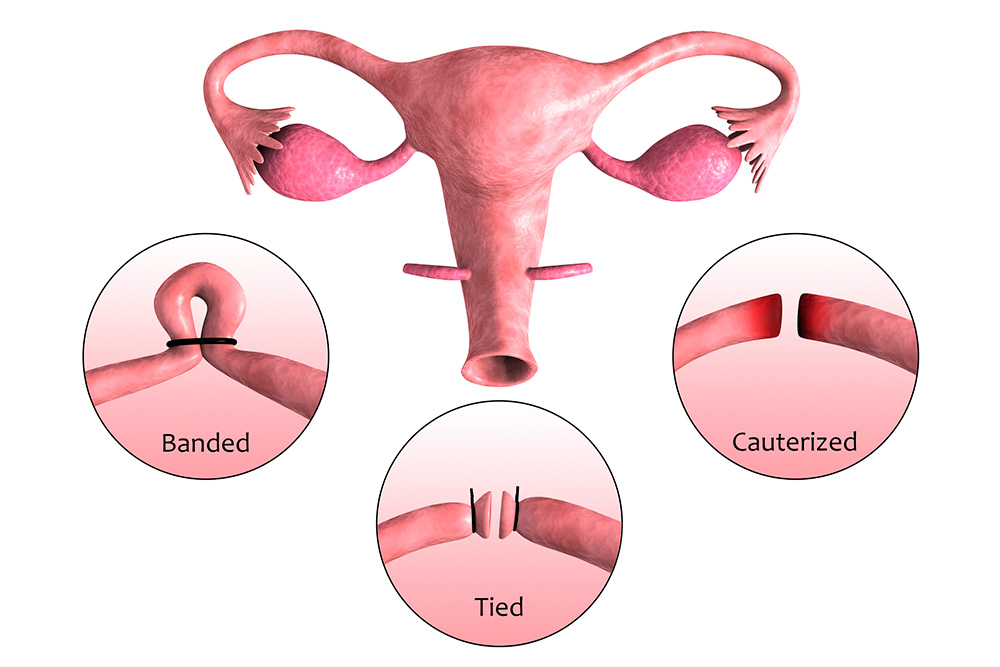
Tubal ligation is a permanent contraception method for women, involving the surgical blocking or sealing of the fallopian tubes. This prevents sperm from reaching the egg, effectively preventing pregnancy.
Reasons for Choosing Tubal Ligation
Many women opt for tubal ligation surgery due to its high effectiveness in preventing pregnancy, its permanence, and the added benefit of reducing the risk of ovarian cancer. While there are other birth control methods, such as birth control pills or intrauterine devices, tubal ligation is a long-term solution that requires no ongoing maintenance.
The Tubal Ligation Procedure
Pre-Operative Preparations
Before undergoing bilateral tubal ligation, patients will have a consultation with their healthcare provider to discuss their medical history, reasons for seeking permanent contraception, and any potential concerns. Pre-operative preparations may include blood tests, a physical examination, and abstaining from food and drink for a specific time before the surgery.
Types of Tubal Ligation Procedures
Keyhole surgery, also known as laparoscopic tubal ligation, is a common method involving a small incision in the abdomen. Other techniques include mini-laparotomy and postpartum tubal ligation, performed shortly after childbirth. Each procedure has its advantages and recovery times, so discussing the best option with a healthcare provider is crucial.
Post-Operative Recovery
After tubal ligation, patients may experience shoulder pain and mild discomfort, which can be managed with prescribed pain medication. Recovery times vary, but most women can return to work within a week. It’s essential to follow post-operative care instructions, such as avoiding heavy lifting, to minimise the risk of complications.
Effectiveness and Reversibility
Success Rate of Tubal Ligation
Tubal ligation is highly effective in preventing pregnancy, with a success rate of over 99%. However, in rare cases, an ectopic pregnancy may occur, which is a serious complication. If a woman becomes pregnant after the procedure, she should seek immediate medical attention.
Potential Complications and Risks
Although tubal ligation is generally considered safe, there are some risks involved. Serious complications, such as infection or damage to the surrounding organs, can occur. It’s essential to discuss these risks with a healthcare provider before deciding on the procedure.
Tubal Ligation Reversal
While tubal ligation is intended to be permanent, some women may seek reversal for various reasons. Reversal involves reconnecting the fallopian tubes, but success rates vary, and the risk of ectopic pregnancy increases. Additionally, the reversal procedure can be costly and is not always covered by insurance.
Emotional and Psychological Considerations
Making an Informed Decision
Deciding on a permanent form of contraception like tubal ligation is a significant decision that should be carefully considered. It’s essential to weigh the benefits, risks, and alternatives before making a choice. Thoroughly discussing the procedure with a healthcare provider and researching the costs involved can help make an informed decision.
Discussing with Your Partner
Tubal ligation is a personal choice, but it can impact relationships, so it’s important to discuss the decision with your partner. Open and honest conversations about family planning and the potential implications of permanent contraception can help ensure that both partners are on the same page.
Support and Counseling Resources
For women considering tubal ligation, seeking support and counselling from healthcare professionals, family, friends, or support groups can provide valuable insights and help ease the decision-making process. Additionally, mental health professionals can offer guidance in coping with the emotional aspects of choosing permanent contraception.
Read more about Vasectomy vs Tubal ligation in our other blog post.

How much does tubal ligation cost in Australia?
The cost of getting your tubes tied in Australia varies depending on factors like the surgeon’s fees, hospital or clinic charges, and geographical location. On average, the procedure can range from $1,500 to $6,000. Private health insurance may cover part or all of the expenses, but it’s essential to confirm coverage with your insurance provider.
What is the best age to get your tubes tied?
There is no definitive “best age” to get your tubes tied, as it depends on an individual’s personal circumstances, family planning goals, and medical history. It’s essential to have a thorough discussion with your healthcare provider to determine if tubal ligation is the right choice for you at any stage of your life.
What age can you get your tubes tied in Australia?
In Australia, there is no specific legal age requirement for tubal ligation. However, medical professionals usually recommend the procedure for women who are at least 18 years old, have completed their family, or have a valid medical reason for seeking permanent contraception.
Does getting your tubes tied stop your period?
No, getting your tubes tied does not stop your period. Tubal ligation involves blocking or sealing the fallopian tubes, preventing sperm from reaching the egg. However, it doesn’t affect the menstrual cycle or the production of hormones that regulate it.
How soon can I have sex after a tubal ligation?
You can typically resume sexual activity within one to two weeks after a tubal ligation, depending on your comfort level and your doctor’s recommendations. However, it’s essential to follow your healthcare provider’s post-operative instructions to ensure proper healing and avoid complications.
How soon is the procedure effective?
Tubal ligation is effective immediately after the procedure. Once the fallopian tubes are blocked or sealed, sperm cannot reach the egg, preventing pregnancy. However, it’s essential to confirm the success of the procedure with your healthcare provider during follow-up appointments.
Can sterilisation be reversed?
In some cases, sterilisation can be reversed through a surgical procedure called tubal ligation reversal. This procedure reconnects the fallopian tubes, potentially restoring fertility. However, the success rates vary, and there is an increased risk of ectopic pregnancy after reversal. It’s also important to note that the reversal procedure can be costly and is not always covered by insurance.