Open-ended, No-scalpel
Vasectomy Services Australia
Safe and Effective Vasectomy Procedure
Are you considering a permanent form of birth control? A vasectomy may be the right option for you. A vasectomy is a safe and effective way to prevent pregnancy and is a popular choice for men who no longer wish to have children. The no-scalpel vasectomy procedure is quick, and straightforward, and can be performed in our Private Day Hospitals or Medical Centres across Australia, including Sydney, Melbourne, Brisbane, Perth, Adelaide, Gold Coast, and more. Most men experience a short recovery time and can return to their normal activities within a few days.
If you are interested in learning more about the vasectomy procedure, keep reading to find out how it works, who it is right for, and what to expect during and after.
What is Vasectomy?
A vasectomy is a surgical procedure for men who have decided not to have more, or any, children. Vasectomy is the only permanent method of contraception for men and has a failure rate of approximately 0.1%. Vasectomy procedures are one of the most commonly performed surgical procedures in Australia, with over 29,000 men getting one each year.
The male vasectomy procedure involves separating the cut end of the tubes that move sperm from the testicles to the penis. After the procedure, ejaculated semen will contain no sperm. Sperm is the component that leads to pregnancy, and after a vasectomy it will be reabsorbed into your body through your tissue instead of being integrated into your semen.

Why Choose MSI Vasectomy
Vasectomies are reliable and extremely effective. Experienced vasectomy surgeons typically have success rates of greater than 99.9%. Other reasons to opt for a vasectomy include:
- It is a one-time cost. Vasectomy is a permanent choice of birth control, which means it is just a one-time expense.
- The procedure is often covered by insurance. Many of our vasectomy clinics across Australia are eligible for private health rebates for vasectomy procedures.
- Does not affect sexual pleasure. A man’s orgasm will be no different than before the vasectomy.
- Minimally invasive. Quick recovery. The MSI No Scalpel Open Ended Vasectomy technique used at MSI Australia causes considerably less tissue trauma than a regular vasectomy. This means a lower risk of infection, less discomfort, faster healing and a speedier overall recovery.
HOW MUCH DOES A VASECTOMY COST IN AUSTRALIA?
Vasectomy Procedure Cost
The cost of a vasectomy procedure in Australia can vary depending on location and whether you use private health insurance. At MSI Vasectomy, we offer competitive pricing and accept private health insurance at many of our locations. For specific pricing information in your area, such as Sydney, Melbourne, Brisbane, or Perth, please contact your nearest MSI clinic.
Choose Your Type of Insurance
- Medicare Only
- Private Health Insurance & Medicare
- No Medicare
Medical Centre
Private Day Hospital
With Intravenous Sedation: From $825**
Intravenous Sedation: Minimal or No Gap*
With Intravenous Sedation: $1,655
Vasectomy Procedure Types
Before considering a vasectomy procedure it’s important to understand that you should consider it an irreversible process. Whilst vasectomy reversal services do exist, we don’t offer this procedure and we advise our patients to treat their vasectomy as non-reversible.
Vasectomy reversals are very expensive, not normally covered by health insurance and do not have a 100% success rate. Vasectomies are for people who are sure they’ve completed their family, or who are certain they don’t want to have children.

Open ended vasectomy
A closed-ended vasectomy blocks both ends of the cut tube either with suture, clip or by diathermy. The closed-ended method used to be the standard procedure for vasectomies. However, it led to some patients experiencing congestive epididymitis (tenderness caused by pressure building up).
An open-ended vasectomy only closes the upper part of the tube, leaving the end connected to the testicle completely open. This allows the sperm to be released within the scrotum, which is not noticeable as the volume is very small. The sperm are naturally reabsorbed and there is less chance of congestive epididymitis and other complications.

No scalpel vasectomy
Before the no scalpel method, many vasectomies would require a scalpel incision and therefore, sutures. A no scalpel vasectomy only requires a single small puncture in the skin, and no stitches. We do this with a specially designed set of forceps. This decreases the chance of infection and minimises the chance of pain.
Some vasectomies may be advertised as a ‘no scalpel, no needle’ procedure. Before booking with one of these practitioners it’s important to ensure that they are doing this with devices approved by the Therapeutic Goods Administration (TGA).
Currently there are no devices capable of delivering a local anaesthetic through the skin that are TGA approved.
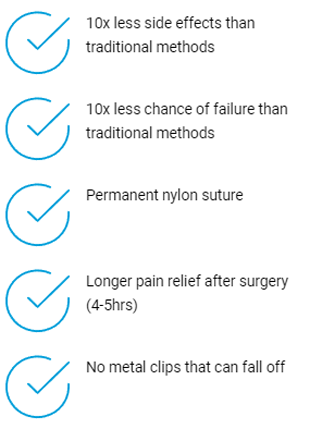
The MSI No Scalpel Open Ended Vasectomy Technique uses an inert permanent suture rather than a metal clip (which can fall off) or a dissolving suture (which can cause inflammation). We also use Bupivacaine local anaesthetic which has a longer duration of action and may protect from chronic post operative pain.

Book Your Vasectomy With Australia's Largest Not-for-Profit Vasectomy Provider
MSI Vasectomy offers expert vasectomy services across Australia, including Sydney, Melbourne, Brisbane, Perth, Adelaide, Gold Coast, and more. With over 20 years of experience and 600,000 satisfied patients, we’re committed to providing high-quality, reliable family planning and vasectomy services.
Anaesthetic Options
At MSI Australia we provide a comprehensive service where both IV sedation (IV) and local anaesthetic (LA) are available. Our LA painless anaesthetic delivery technique means many patients report experiencing little to no pain when the local anaesthetic is injected.
Anyone can choose to have IV Sedation for their vasectomy and many men simply prefer to be “knocked out” as they know they will not handle being awake for the procedure well.
Other men may have had previous inguinal hernia or scrotal surgery in which case we recommend them to have IV sedation as there is a chance that old scar tissue will make the vasectomy under LA difficult and may even mean the LA operation is postponed to a later date for the needed IV sedation. For all men who have had a vasectomy in the past, we insist on them having IV sedation for the same reasons.

Why Choose MSI For Your Vasectomy?
For the last 20 years, we at MSI Vasectomy have championed the rights of Australians to access high-quality, reliable family planning and vasectomy services. In that time, over 600,000 men have trusted us with their sexual and reproductive health needs.
Our 4 Key Points of Difference are:
- We are the largest vasectomy provider in Australia
- High quality, standardised MSI ‘No-Scalpel Open-Ended’ technique with all our vasectomy doctors
- Minimal or No GAP with Private Health Insurance and from $590 out of pocket with Medicare (available at certain locations)
- Local anaesthetic and IV sedation options (available at certain locations)
Meet Dr Justin Low
National Director of Vasectomy Services
Justin’s current role is National Director of Vasectomy Services at MSI Vasectomy Australia which involves education, training and maintaining vasectomy surgical standards across the country.
Justin received his medical degree from the University of Sydney in 1987 and completed the RACGP Family Medicine Program (FMP) in 1991. He became a Fellow of the Royal Australian College of General Practitioners in 1993.
Justin presents to General Practice groups regularly around the country on the topic of vasectomies and has been interviewed on ABC Radio National, Sydney Morning Herald “Good Weekend”, Men’s Health Magazine and Channel 9’s “Today” morning show.

If you have any more questions about our vasectomy procedure don’t hesitate to contact us today. In the meantime please find below our most frequently asked questions about vasectomies.
Is it painful to have a vasectomy?
No, a vasectomy is usually not very painful. The procedure is typically performed under local anaesthesia or IV sedation and most men report feeling only mild discomfort or pressure during the procedure, but severe pain is rare. After the procedure, some men may experience some swelling, bruising, or mild pain or discomfort, but these symptoms usually go away within a few days.
How long does it take a man to recover from vasectomy surgery?
Most men can return to their normal activities within a few days after a vasectomy. However, it is recommended to avoid strenuous physical activity for two weeks after the procedure to allow the body to heal properly.
Does a vasectomy protect against sexually transmitted infections?
No, a vasectomy does not protect against sexually transmitted infections (STIs). It is only a method of contraception and does not provide any protection against STIs. Condoms are the only effective way to reduce the risk of STIs.
Can a vasectomy be reversed?
Yes, it is possible to reverse a vasectomy, but the success rates can vary. The procedure involves rejoining the severed ends of the vas deferens (the tubes that carry sperm), and is more complicated than a vasectomy. The success of the procedure depends on various factors, such as the length of time since the vasectomy, the surgical technique used, and the age and fertility of the man.
Does a vasectomy make prostate cancer more likely?
There is currently no evidence to suggest that having a vasectomy increases the risk of prostate cancer. Several large studies have investigated this question, and the results have been inconclusive.
Is it similar to female tubal ligation?
Vasectomy and tubal ligation are both surgical procedures that are used to achieve permanent contraception. However, they are quite different in terms of how they are performed and their risks and benefits. Vasectomy surgery is typically a simpler and less invasive procedure than tubal ligation, and it has a lower risk of complications.
Is in vitro fertilisation possible after vasectomy?
Yes, in vitro fertilisation (IVF) is an option for couples who want to have a child after the man has had a vasectomy. In this procedure, the woman’s eggs are fertilised with the man’s sperm in a laboratory, and the resulting embryos are transferred to the woman’s uterus. However, IVF can be expensive and is not always successful.
Can I get a vasectomy in Sydney/Melbourne/Brisbane?
Yes, MSI Vasectomy offers no-scalpel vasectomy services in major cities across Australia, including Sydney, Melbourne, Brisbane, Perth, Adelaide, and more. Contact your nearest MSI clinic for more information.
Does the vasectomy cost the same across Australia?
Vasectomy costs can vary depending on location and whether you use private health insurance. For specific pricing information in Melbourne, Sydney, Brisbane, or other Australian cities, please contact your local MSI clinic.
How is a vasectomy performed in Australia?
At MSI Vasectomy, we use the no-scalpel, open-ended technique for all our vasectomy procedures across Australia. This method is less invasive and typically results in faster recovery times.
What's the vasectomy failure rate?
The vasectomy failure rate is extremely low, approximately 0.1%. This makes vasectomy one of the most effective forms of permanent contraception available.
Is the "male snip" the same as a vasectomy?
Yes, “male snip” is a colloquial term for a vasectomy. At MSI, we perform the no-scalpel vasectomy, which doesn’t actually involve any snipping.
How long does a vasectomy procedure take in Australia?
At MSI Vasectomy clinics across Australia, including Sydney, Melbourne, and Brisbane, the entire vasectomy process typically takes no more than 15 minutes.
What's the best way to prepare for a male vasectomy?
Preparation for a male vasectomy at MSI clinics involves a pre-procedure consultation, understanding the process, and following your doctor’s instructions. This may include stopping certain medications and arranging time off work for recovery. Review our patient information for more details on our vasectomy process.
What should I expect during my vasectomy procedure?
At MSI Vasectomy clinics, you’ll receive either IV sedation or local anaesthetic. The doctor will make a small incision, seal the vas deferens, and apply a small dressing. The procedure is quick and generally completed within 15 minutes.
Is a vasectomy painful?
Vasectomies are not painful during the procedure due to anaesthesia. Some men may experience mild discomfort afterwards, which is typically manageable with over-the-counter pain relief.
When can I return to work after a vasectomy in Australia?
For desk jobs, you can usually return to work the day after your procedure. For physically demanding jobs, you may need a week off or light duties. MSI can provide medical certificates if needed.
How long should I avoid physical activity after a vasectomy in Australia?
After a vasectomy, avoid strenuous activities for 1 week, non-contact sports for 2 weeks, and contact sports for 1 month. Cycling has specific timeframes depending on the type. For more information on exercising after a vasectomy, read our informative blog.
When can I resume sexual activity after a vasectomy?
After a male vasectomy, abstain from sex for the first week. Use contraception for 3 months post-procedure until a clear semen test confirms the absence of sperm. Remember, vasectomies don’t protect against STIs.
Can I still have children after a vasectomy?
A vasectomy is a permanent method of birth control. After vasectomy surgery, sperm is no longer present in the ejaculate, making natural conception impossible. If you are considering having more children in the future, it’s important to think carefully before proceeding. While vasectomy reversals exist, they are complex, not always successful, and are often not covered by insurance. Some couples may explore options like IVF after vasectomy to conceive.
What are the side effects of a vasectomy?
The no-scalpel vasectomy is a minimally invasive procedure, and side effects are usually mild. Some men experience temporary discomfort, swelling, or bruising around the surgery area. Rare side effects include infection or chronic pain, but these risks are significantly reduced when the vasectomy is performed by an experienced vasectomy doctor. Most men recover within a few days and can return to regular activities shortly after the procedure.
What are the benefits of having a vasectomy?
A vasectomy offers a permanent and highly effective form of birth control with a success rate of over 99.9%. The procedure is simple, especially with the no-scalpel vasectomy technique, which reduces recovery time and the risk of complications. It’s a one-time procedure with no long-term side effects on sexual function or health. Vasectomy surgery is also cost-effective in the long run, compared to ongoing contraceptive methods.
What are the disadvantages of getting vasectomy surgery?
The main disadvantage of a vasectomy is its permanent nature. While vasectomy reversals exist, they are not guaranteed and can be expensive. There is also a small risk of complications such as infection, bleeding, or chronic pain, although these are rare, especially with the no-scalpel vasectomy method. A vasectomy does not protect against sexually transmitted infections (STIs), so other protection methods may still be necessary.
How effective is a vasectomy?
A vasectomy is one of the most effective forms of permanent contraception, with a success rate of 99.9%. However, it’s important to note that sperm can still be present in the semen for a short time after the procedure. It can take up to 3 months and several ejaculations to clear out the remaining sperm. A follow-up semen analysis is necessary to confirm the vasectomy’s success before discontinuing other forms of birth control.
How does a no scalpal vasectomy work?
In a no-scalpel vasectomy, a small puncture is made in the scrotum instead of a traditional incision, reducing recovery time and the risk of complications. The sperm produced after the procedure is safely reabsorbed by the body.
What should I expect after having vasectomy surgery?
After a vasectomy, most men experience mild discomfort and swelling, which typically resolves within a few days. It’s important to rest and avoid strenuous activities for two weeks following the procedure. You will need to use alternative birth control until a follow-up test confirms there are no sperm in your semen. The no scalpel vasectomy technique allows for a quicker recovery and lower risk of infection compared to traditional methods.
What happens to sperm after a vasectomy?
After a vasectomy, your testicles continue to produce sperm, but the sperm is absorbed by the body instead of being mixed with semen. The sperm is naturally broken down and reabsorbed. This is a normal process and does not affect your overall health or sexual function. The no scalpel vasectomy technique ensures minimal disruption to surrounding tissues, further reducing the risk of complications.
Will I last longer during sex after a vasectomy?
A vasectomy does not directly affect your ability to last longer during sex. The procedure only stops sperm from being present in the ejaculate and does not impact your sexual performance, desire, or sensation. Most men report no changes in their sexual experience after vasectomy surgery.