Table of Contents
In our latest blog post, we discuss the key aspects of castration vs vasectomy, two surgical procedures that impact male fertility. We explore how these procedures affect the prostate gland, vas deferens, and testosterone production, as well as touch upon topics such as prostate cancer, hormones, and male sterility.
Understanding Castration vs Vasectomy
Castration is the surgical removal of one or both testicles, also known as the testes. This procedure called a bilateral orchiectomy, is usually performed in males to reduce testosterone levels, which can help treat prostate cancer or other health conditions.
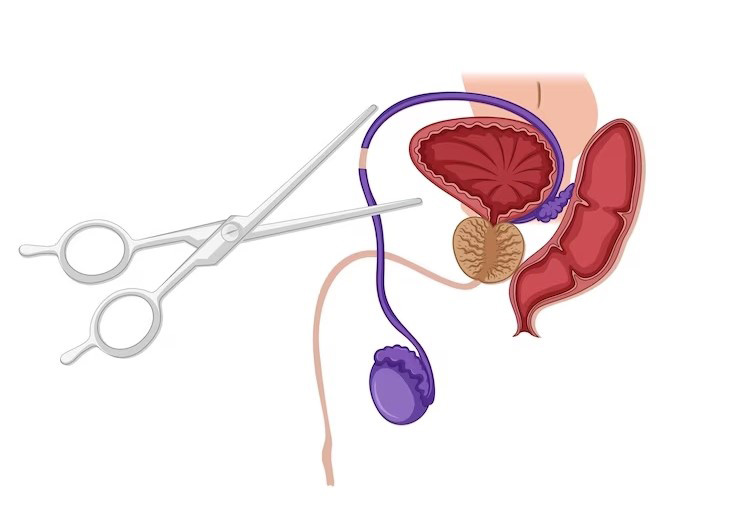
Vasectomy, on the other hand, is a surgical procedure that interrupts the vas deferens, the tubes that carry sperm from the testicles. This procedure is performed to achieve male sterility without affecting sex hormones or testosterone production, making it a more favourable choice for many men.
The Medical Procedures
During a castration, the surgeon removes the testicles, which are responsible for producing sperm and male hormones like testosterone. This procedure results in permanent sterility and a significant decrease in testosterone levels.
Vasectomy involves interrupting the vas deferens, the tubes through which sperm travels from the testicles to the prostate gland. This prevents sperm from mixing with semen, rendering a male sterile without affecting his sex drive or testosterone production. As a less invasive procedure, vasectomy is often preferred by men seeking permanent contraception.
Key Differences: Vasectomy vs Castration
There are a number of key differences between castration and vasectomy:
Surgical Techniques
The main difference between these surgical procedures is the extent of the intervention. Castration involves the complete removal of the testes, while vasectomy targets the vas deferens, leaving the testicles intact. This makes vasectomy a less invasive and more appealing option for males seeking sterilisation.
Impact on Fertility
Both castration and vasectomy lead to male sterility, but their effects on fertility differ. Castration results in the complete loss of sperm production, while vasectomy merely prevents sperm from being ejaculated.
This means that, after a vasectomy, sperm is still produced but cannot reach the prostate gland or be released during ejaculation. Due to this, vasectomy is often considered a more favourable approach for males who want to maintain their hormone levels.
Hormonal Changes
Castration causes a significant decrease in testosterone levels, as the testicles are responsible for producing this male hormone. This can lead to various side effects, such as reduced sex drive, muscle loss, and mood changes.
In contrast, after a vasectomy, the testes continue to produce testosterone as the testicles remain functional. This hormonal stability makes vasectomy a more attractive option for men considering permanent contraception.
Recovery and Aftercare
Recovery times and aftercare requirements also differ between these procedures. Castration typically involves a longer recovery period and may require additional support, such as hormone replacement therapy, to manage side effects.
Vasectomy recovery is usually quicker, with most males resuming normal activities within a week, further emphasising the appeal of vasectomy over castration.
Benefits and Risks of Castration and Vasectomy
Even though they achieve the same outcome, the benefits and risks of castration vs vasectomy are different:
Advantages of Castration
Castration is effective for treating certain medical conditions, such as prostate cancer, by reducing testosterone levels. In some cases, chemical castration using medications is employed as an alternative to surgical removal of the testes.
Advantages of Vasectomy
Vasectomy is a popular choice for permanent male sterilisation due to its minimal impact on sex drive, testosterone production, and overall health. It is a relatively simple procedure with a high success rate and low risk of complications. Men often opt for vasectomy as it allows them to maintain their hormonal balance and enjoy their regular lifestyle without the worry of unwanted pregnancies.
Potential Risks and Complications
As with any surgical procedure, both castration and vasectomy carry potential risks, such as infection, bleeding, or adverse reactions to anaesthesia. Castration may lead to long-term side effects, such as decreased bone density, weight gain, and mood changes, while vasectomy can occasionally result in chronic pain or sperm granulomas.
However, the risks associated with vasectomy are generally fewer and less severe than those related to castration, further solidifying its position as the more favourable option for most men.

Summary
While both methods serve their purposes, vasectomy is the more favourable option for men seeking permanent contraception due to its less invasive nature and minimal impact on sex drive and testosterone production.
Remember it’s crucial for you to consult with a medical professional if you’re considering either procedure, weighing the benefits and risks, and taking into account your personal goals and lifestyle factors before making a decision.
How effective are these procedures?
Both castration and vasectomy are highly effective methods of achieving their intended outcomes. Vasectomy is considered one of the most reliable forms of permanent male contraception, with a success rate of over 99%. Castration is effective at reducing testosterone levels, which can help treat specific medical conditions.
Can they be reversed?
While vasectomy reversal is possible in some cases, the procedure is not always successful, and fertility may not be restored. Castration is irreversible, as the testicles cannot be replaced or regenerated.
What are the long-term effects?
The long-term effects of castration include decreased testosterone levels, which can lead to various physical and emotional changes. Vasectomy, on the other hand, does not typically have long-term effects on testosterone levels, sex drive, or overall health, making it a more attractive option for men seeking permanent contraception.
Does a vasectomy offer immediate protection against pregnancy?
A vasectomy does not provide immediate protection against pregnancy. Following the procedure, sperm may still be present in the vas deferens and can take several months to be cleared out. It is essential for men to continue using other contraceptive methods until a semen analysis confirms the absence of sperm.
How does the cost of castration compare to the cost of a vasectomy?
The cost of vasectomy and castration can vary depending on factors such as location, healthcare providers, and insurance coverage. Generally, vasectomy tends to be a more affordable option as it is a simpler, outpatient procedure with fewer associated costs. Castration, on the other hand, is more invasive and may require hospitalisation, leading to higher costs.